Head-to-Toe Assessment Checklist: A Complete Guide for Nurses
Stay organized and confident in your assessments. This guide walks you through the head-to-toe assessment checklist and provides a free PDF for everyday practice.
September 29, 2025
12 min. read

The head-to-toe assessment is one of the first skills every nurse learns, and it’s one you’ll return to throughout your career. It’s your structured roadmap for understanding a patient’s overall health, establishing a baseline, and catching subtle changes that can signal complications.
At first, it can feel like a lot to keep track of. There are so many body systems, details, and patient factors competing for your attention. But with practice, these steps become second nature—and having a head-to-toe assessment checklist can make the process less daunting and more consistent.
In this guide, we’ll walk through what a head-to-toe assessment is, why it matters, and how to prepare. Plus, we've provided a free checklist to help make your nursing assessments thorough, efficient, and patient-centered.
What is a head-to-toe assessment?
A head-to-toe assessment is a comprehensive, systematic evaluation of the patient, moving from general observations to a detailed review of each body system.1
The purpose is simple: gather a full picture of the patient’s health so you can identify needs, prioritize care, and communicate findings with the healthcare team. This exam is not just about checking boxes—it’s about establishing a thorough understanding of a patient's overall health status and using that information to make safe, effective decisions.
You’ll typically perform a head-to-toe assessment:
At admission or start of care to create a baseline.
At the start of your shift or during a handoff to ensure continuity.
When resuming care after hospitalization or a significant event.
During home health or long-term care visits to monitor ongoing status.
With recertifications or routine reassessments to capture changes over time.
Whenever a patient’s condition changes or new symptoms appear.
At discharge to confirm stability and provide final discharge instructions and education.
If a patient is unstable, you may need to begin with a focused assessment that zeroes in on the most critical system, then return to the full exam once the situation is stabilized.
Why the head-to-toe assessment matters for nurses
The head-to-toe assessment may seem routine, but it’s the foundation of safe and effective nursing care. Here’s why it matters:
Patient safety: Catch early warning signs, such as changes in mental status, subtle respiratory issues, or skin breakdown, before they escalate into bigger problems.
Clinical decision-making: Use your findings to adjust medications, escalate concerns, and plan interventions with confidence.
Patient-centered care: Deliver care that reflects each patient’s unique needs, preferences, and priorities.
Monitoring outcomes: Track progress toward goals—whether healing a wound, stabilizing heart failure, or improving ambulation—and update the plan of care at the right time.
Communication: Share clear, consistent information with the healthcare team to keep everyone aligned.
Confidence and efficiency: Build your confidence, strengthen clinical judgment, and avoid missed details with a structured approach.
In short, the head-to-toe assessment is where quality care begins, and the right tools can make all the difference. To support your practice, download our free Head-to-Toe Assessment Checklist PDF below. This printable resource is designed to help you keep your exams organized, consistent, and reliable.
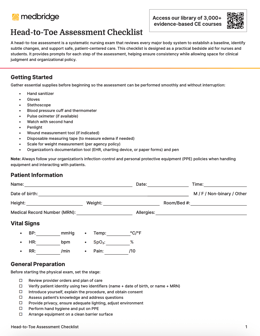
Head-to-Toe Assessment Checklist
Preparing for a head-to-toe assessment
Before you pick up your stethoscope, set yourself and your patient up for success. Preparation isn’t just about equipment. It’s about creating a comfortable, safe, and respectful environment where the patient feels at ease and you can perform a thorough exam.
Keep in mind that assessment begins before the hands-on exam. As a nurse, you constantly listen, observe, and notice subtle cues (such as mood, speech, posture, environment, and ambulation) that shape your clinical judgment.
Here are some essentials to cover:
Review the care plan
Know your patient’s diagnoses, provider orders, and current medications. This helps you focus your assessment on areas that may be higher risk or require closer monitoring.
Make the environment comfortable
Ensure the room is well-lit, quiet, and private. Adjust the temperature if necessary. Small touches, like drawing a curtain or dimming overhead lights, can make a big difference in how patients experience the exam.
Build rapport
Introduce yourself, explain what you’ll be doing, and ask how they prefer to be addressed. Many patients are anxious about physical exams, and taking a minute to explain the process can lower stress and build trust.
Practice infection control
Wash your hands and follow your organization's PPE guidelines. Infection prevention protects both you and the patient.
Core methods of physical examination
Every head-to-toe exam relies on four core methods of physical examination. Used together, they help you build a clear picture of your patient’s health.
1. Inspection
Always the first step. Use your eyes, and sometimes your sense of smell, to note color, shape, movement, posture, and overall appearance. The skin is especially important—look for breakdown, bruising, changes in color, moisture, and turgor that can signal systemic or localized problems. You’ll also observe nonverbal cues like facial expressions, breathing effort, and overall hygiene, which can provide meaningful context before you touch the patient.
2. Palpation
Use your hands to detect abnormalities such as tenderness, swelling, or differences in texture. Light palpation helps you assess surface structures and skin moisture, while deeper palpation can give information about organ size, consistency, and the presence of masses.
3. Percussion
Tapping the body produces vibrations that help identify whether underlying tissue is air-filled, fluid-filled, or solid. This method is especially valuable in assessing the lungs and abdomen, where differences in sound can reveal consolidation, effusion, or organ enlargement.
4. Auscultation
Use your stethoscope to listen carefully to heart, lung, and bowel sounds. Auscultation can reveal murmurs, crackles, wheezes, or abnormal bowel activity—findings that might otherwise go unnoticed. Direct auscultation (listening with your ear) is less common but useful in some settings.
Nursing head-to-toe assessment checklist
Now that you’ve reviewed the core methods, it’s time to put them into action. A complete head-to-toe assessment should follow a structured flow so no detail is missed. Here’s what your checklist should cover:1
General survey and vitals
Start with a broad impression of the patient’s overall condition.
Observe appearance, posture, hygiene, and orientation.
Take baseline vitals: blood pressure, heart rate, respiratory rate, temperature, oxygen saturation, and pain rating.
Obtain a baseline weight and note height at admission or start of care.
Neurological and psychosocial
Assess cognition and function to establish a baseline.
Note speech clarity, mood, and mental status.
Check orientation to person, place, and time.
Assess handgrip strength, sensation, and coordination.
Watch for confusion, anxiety, or changes from prior assessments.
HEENT (Head, eyes, ears, nose, throat)
Work systematically through each area.
Inspect head and scalp for shape or lesions.
Check pupils for reaction, eye movements, and vision.
Assess hearing, nasal patency, and sinuses.
Inspect oral cavity, mucous membranes, teeth, and swallowing ability.
Cardiovascular and respiratory
Monitor circulation and oxygenation.
Listen to heart sounds in all landmarks.
Check peripheral pulses and capillary refill.
Inspect chest symmetry and respiratory effort.
Assess for dependent edema in the feet, ankles, and legs; grade and measure when present.
Auscultate lung sounds front and back.
Abdomen and gastrointestinal
Evaluate both function and comfort.
Inspect contour and symmetry.
Auscultate bowel sounds in all quadrants.
Palpate lightly for tenderness or distention.
Ask about appetite, elimination, or nausea.
Musculoskeletal and extremities
Focus on mobility and strength.
Assess range of motion, balance, and gait.
Inspect for swelling, deformities, or pain.
Check for edema or tenderness in extremities.
Skin, hair, nails
Skin findings often reveal important health clues.
Inspect color, temperature, moisture, and turgor.
Check for lesions, rashes, wounds, or pressure injuries.
Evaluate nail shape, color, and capillary refill.
Be thorough in vulnerable areas such as heels, feet, buttocks and the sacral region.
Don’t forget to download the full Head-to-Toe Assessment Checklist PDF for a printable, bedside-ready guide. Each section includes space for notes, making it easy to document findings and track changes for every patient.
Going beyond the physical exam
A thorough head-to-toe assessment always extends past body systems. Along with physical findings, you should also assess mobility, emotional well-being, and the safety of the patient's environment. Challenges in these areas highlight risks and priorities for care planning.
A thorough head-to-toe assessment doesn’t stop at physical findings—it also takes into account the broader factors that influence recovery and long-term outcomes:
Functional status: Can the patient transfer safely, ambulate independently, and complete activities of daily living (ADLs) such as dressing, eating, and bathing? Limitations here often guide rehabilitation priorities and care planning.
Safety and environment: Are there risks in the patient’s surroundings (like poor lighting, clutter, or missing mobility supports) that increase fall risk? In hospital settings, are call lights, bed rails, and aids positioned and used appropriately?
Psychosocial health: How is the patient coping emotionally? Are there signs of stress, anxiety, or withdrawal? Do they have reliable support systems, whether family, caregivers, or community resources?
Medication reconciliation and review: Verify an accurate medication list, ensure medications are appropriate, taken as prescribed, and free of interactions or side effects that impact safety, function, or quality of life.
Considering these dimensions provides context that body system assessments alone can’t. When you integrate functional, environmental, and psychosocial insights, you help create care plans that are holistic, realistic, and truly patient-centered.
Case examples: Using the head-to-toe assessment checklist in practice
1. Managing congestive heart failure at home
During a routine home health visit, an RN uses the head-to-toe checklist to assess a patient with congestive heart failure. Findings include:
General survey and vitals: A four-pound weight gain since the last visit and elevated blood pressure.
Cardiovascular and respiratory: Bilateral ankle edema and fine crackles at the lung bases.
Functional status: Increased shortness of breath after minimal exertion, a change from baseline.
Because the checklist ensured a structured and consistent review, the nurse documented all findings clearly and promptly communicated them to the provider. Medications were adjusted the same day, preventing worsening fluid overload and a likely hospitalization.
2. Preventing skin breakdown in long-term care
In a long-term care facility, a nurse performs a scheduled head-to-toe assessment for a resident with limited mobility. Guided by the checklist, the nurse notes:
General survey and vitals: The resident appears fatigued but hemodynamically stable.
Skin, hair, nails: Early redness over the coccyx and heels, not present at the last assessment.
Because the checklist prompted a full skin check, these subtle changes were caught early. Interventions—including repositioning every two hours, applying barrier creams, and ordering a specialty mattress—were initiated immediately, preventing a pressure injury from developing.
3. Identifying fall risk during admission
On admission to a hospital unit, a nurse uses the checklist to evaluate an older adult admitted with pneumonia. The structured approach highlights multiple concerns:
General survey and vitals: Orthostatic hypotension with dizziness on standing.
Neurological and psychosocial: Oriented, but requires frequent cues for time and situation, suggesting mild cognitive impairment.
Musculoskeletal and extremities: Reduced lower extremity strength and unsteady gait requiring assistance.
With fall risk identified early, the nurse implemented immediate interventions such as a fall risk armband, non-slip socks, a bed alarm, and frequent rounding. These precautions reduced the likelihood of a preventable fall during hospitalization.
Tips for a better head-to-toe assessment
Even with experience, it’s easy to miss details when you’re busy or rushed. Keeping these tips in mind will help you stay thorough during every assessment:
Use the head-to-toe assessment checklist. A structured guide keeps you regimented and prevents missed steps, especially when time is limited.
Don’t skip neuro. Neurological checks are often overlooked, but provide critical information about patient status.
Listen everywhere. Auscultate all lung fields—front, back, and sides—to avoid missing subtle abnormalities.
Check the skin. Pressure points and skin integrity can reveal problems early if inspected consistently.
Be specific in your notes. Replace vague phrases like “lungs clear” with clear, detailed documentation.
Communicate openly. Explain what you’re doing and why to build trust and cooperation with patients.
Compare both sides. Look for symmetry in strength, sensation, and movement—differences can signal underlying issues.
Stay curious. If something feels “off,” dig deeper or escalate concerns rather than dismissing them.
From checklist to confidence
The head-to-toe assessment may seem like a long list of tasks at first, but with practice, it becomes second nature—an ingrained part of how nurses think and care for patients. Most clinicians find that, over time, they assess continuously, not just during the exam itself. By pairing your clinical judgment with a structured checklist, you can ensure assessments are thorough, consistent, and patient-centered to provide safe and effective care every time.
Don’t forget to download the free Head-to-Toe Assessment Checklist PDF to stay organized at the bedside, and explore Medbridge's Clinical Procedure Manual for step-by-step guidance, video demonstrations, and expert-reviewed resources to support excellence at the point of care.
References
Ernstmeyer, K., & Christman, E. (Eds.). (2021). Appendix C – Head-to-Toe Assessment Checklist. In Nursing Skills. Open Resources for Nursing (Open RN). Chippewa Valley Technical College. National Library of Medicine Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK593191/